|
PROCEDURES
Inpatient
/ Outpatient
INPATIENT
PROCEDURES
Dr.
Fayaz Shawl has devoted his career to the very latest
in cardiovascular innovations, advancements and patient
procedures. The following inpatient procedures are
all performed in exceptional well-equipped facilities
along with a highly qualified team of nurse/nurse
practitioners, technicians and a medical support staff
specifically trained in cardiovascular care. Please
contact our team with any
questions and we will be happy to assist you with
any inquiries. The highlighted inpatient procedures
are the most common and follow graphical illustration
and/or a summary of the procedure. If you would like
more information on a specific procedure that is not
highlighted, contact our offices directly.
Coronary
Balloon
Angioplasty
Coronary Stenting
Directional Atherectomy
Rotoblation
Rotational Atherectomy
Brachytherapy
High Risk/Inoperable CPS supported angioplasty
Hybrid (MID CAB - LIMA/RIMA + angioplasty)
Excimer Laser
Front Runner cutter for CTO
Percutaneous Cardiopulmonary Bypass
Support - PCPS (High Risk / Waiting for transplant
/ In Cardiac Arrest)
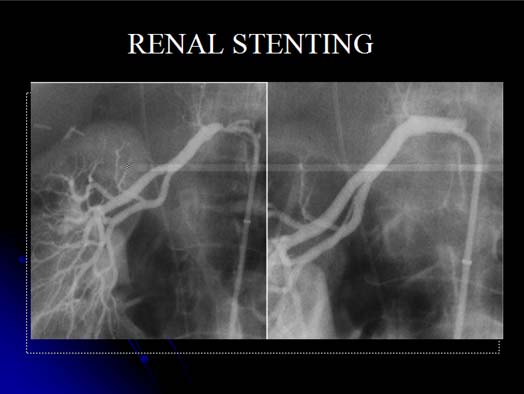
Renal (Kidney) Artery
Stenting
Valvuloplasty
Mitral
Aortic
Pulmonary
Investigational
Cartoid Stenting
Endoluminal Grafting
Percutaneous Aortic Valve Replacement
Cell Regeneration
PTMR
Pericardial Window
Intracranial Angioplasty
Cell Regeneration for CHF
Percutaneous - bypass (vein-arterial conduit)
Distal protection
Acute stroke intervention
VSD - closure
Alcohol Septal Ablation
HOCM
Peripheral
Subclavian
Renal
Lliac
Superficial femerol artery
Infrapopliteal
Aortic Stenting
AAA Endovascular repair
Cell-embolization for aneurysms and fistula
PFO Closure
ASD Closure
Balloon Angioplasty
- (PTCA or Percutaneous Transluminal Coronary Angioplasty)
is a procedure in which a small balloon-tipped catheter
is placed into the artery where there is a narrowing.
The balloon is inflated at the blockage to push the
plaque and fatty deposits against the artery wall.
The balloon is then deflated and removed, allowing
blood to flow without difficulty.
[back]
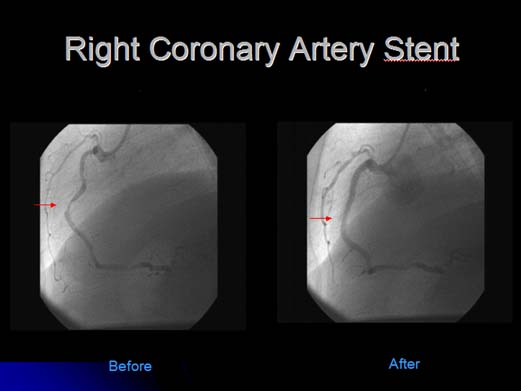
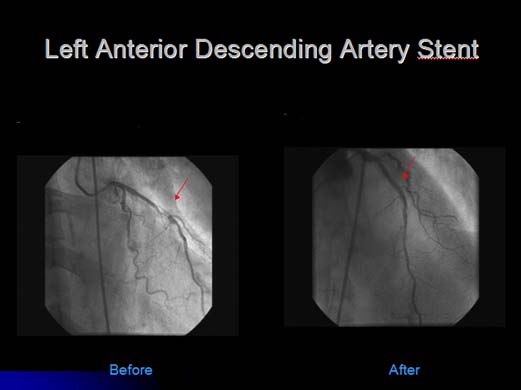
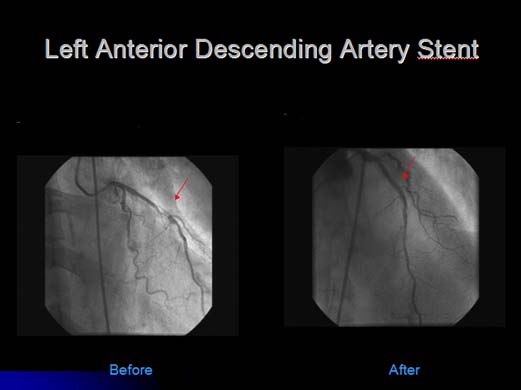
Coronary Stenting
- In
about 70-90% of all balloon angioplasty procedures
a stent is also used. A stent is a tiny metal mesh
tube that is inserted into a narrowed artery by a
balloon- tipped catheter. When the balloon is inflated
the stent opens out to the size of the artery. The
balloon is then deflated and removed while the stent
remains in place. This provides support for the arterial
wall, keeping the artery open. Some stents are self-expanding
and do not require a balloon to open them.
[back]
Directional
Atherectomy
- A procedure in which fat deposits and plaque
are removed by shaving them from the walls of the
artery using a small "cutting" device. This procedure
is usually followed by a balloon angioplasty to squeeze
the remaining plaque against the wall of the artery
and smooth out the edges. A stent may also be used
to help keep the artery open.
[back]
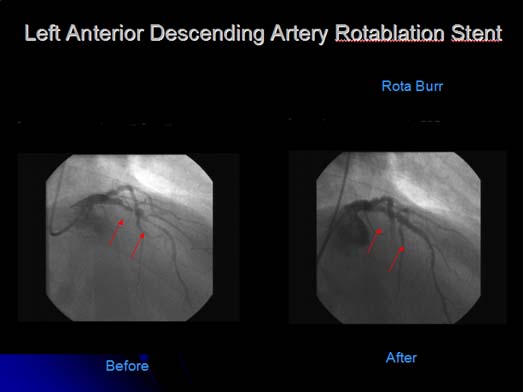
Rotoblation -
A procedure in which a catheter with a rough
diamond-coated tip is inserted into the narrowed artery.
This tip spins at high speeds grinding the hardened
plaque creating an opening. This procedure may be
followed by balloon angioplasty and sometimes a stent,
to smooth the edges and keep the artery open.
[back]
Hybrid
(MID CAB - LIMA/RIMA + angioplasty) - This is
an "integrated minimally invasive approach" or "hybrid
procedure". The only advantage of conventional bypass
surgery is excellent outcome with arterial conduits
like LIMA, RIMA, radial or gastroepiploic vessels.
We can use these conduits by minimally invasive (MIDCAB)
surgery. In patients with multiple vessel disease,
instead of conventional CABG, we use combined MIDCAB
and percutaneous intervention.
[back]
Excimer Laser -
This procedure removes blockages (plaque) from the
artery with laser energy. The laser energy is sent
through a metal tipped catheter and the blockage is
vaporized and cleared from the artery.
[back]
Percutaneous Cardiopulmonary
Bypass Support - PCPS (High Risk / Waiting for
transplant / In Cardiac Arrest) (PCPS) is a highly
specialized procedure developed by Dr. Shawl especially
for the "high-risk" patient. PCPS provides assistance
to the heart during cardiac arrest and, in a controlled
setting, during high-risk coronary intervention. Click
here to access videos about this procedure.
[back]
Renal (Kidney)
Artery Stenting -
Renal artery blockages result from a build
up of plaque, which narrows the artery. This may lead
to high blood pressure and total blockages can lead
to kidney failure. The renal arteries can be treated
the same as other peripheral arteries. The stent is
placed with a balloon-tipped catheter. This is introduced
into the patient by a needle puncture into the groin
site (femoral artery). The balloon is removed leaving
the stent in place to keep the artery open.
[back]
Valvuloplasty -
A non-surgical treatment for heart valve stenosis
(a narrowing of the heart valve). During this procedure
the narrowed valve is stretched open by a balloon-tipped
catheter. The balloon is inflated until the valve
is expanded; then the balloon is deflated and removed.
[back]
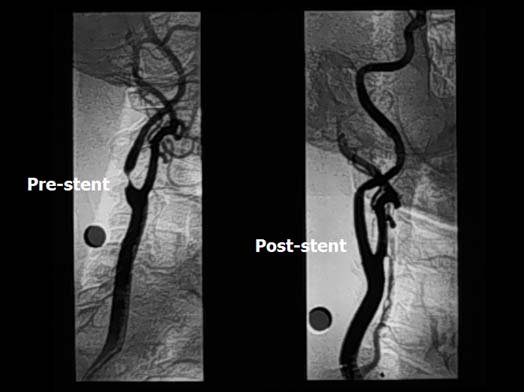
Cartoid Stenting
- The carotid arteries are located on each side of
the neck and supply blood to the brain. Carotid artery
stenting is done to prevent future strokes in people
with a blockage in the carotid artery. This is a non-surgical
procedure in which a metal mesh cylinder is inserted
into the carotid artery by a balloon-tipped catheter.
The balloon is inflated which expands the stent to
the artery wall thus opening the blood vessel. The
balloon is deflated and removed and the stent remains
in place to keep the artery open.
[back]
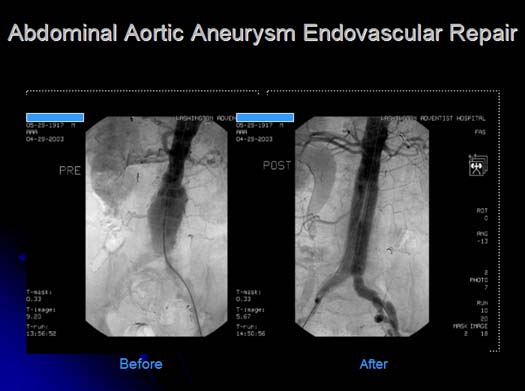
Endoluminal
Grafting - This procedure is done to treat aortic
aneurysms. Aortic aneurysms are a weakening of the
arterial wall in the aorta, which is located in the
abdomen. This arterial wall becomes dilated (like
a balloon) and may rupture. Endoluminal grafting is
a non-surgical procedure in which a graft is placed
inside the aneurysm through a tube in the groin (femoral
artery). This graft is attached to the wall of the
artery above and below the aneurysm. Blood will then
flow through the graft away from the weakened arterial
wall allowing the aneurysm to shrink.
[back]
PTMR Percutaneous Transluminal
Myocardial Revascularization - There are many
patients who because of small size vessels or diffuse
disease are not good candidates for percutaneous interventions
or bypass surgery. These patients become severely
limited because of incapacitating angina. PTMR
can provide these patients with symptomatic relief
of angina. In some animals, like crocodiles and alligators,
the blood flow to the heart muscle is directly from
the LV chamber via small channels. Based on this knowledge,
Dr. Mirhoseini created channels in human hearts using
laser energy. Over the last few years other surgeons
have created similar laser channels directly into
the heart muscle with objectively evident beneficial
effects. However the surgical method is more invasive
and is associated with 10-19% mortality. Now, using
catheter-based technology, we are able to create channels
from inside the chamber of the heart into the LV muscles.
Dr. Fayaz Shawl performed the first PTMR in the human
heart in India without any complications. Today, Dr.
Shawl performs PTMR in the U.S. with FDA IDE approval
and has done a number of cases with great success
and promising results.
[back]
Alcohol Septal
Ablation HOCM - A technique in which ethanol
is injected directly to the heart in order to treat
thickening heart muscle cells in patients diagnosed
with Hypertrophic Obstructive Cardiomyopathy. The
alcohol septal ablation procedure begins with physicians
inserting a small catheter into an artery in the groin,
and then threading it to the heart. The treatment
decreases the thickened muscle that divides the heart's
two chambers so that it can retract, restoring normal
function. After treatment, patients will notice significant
improvement almost immediately.
[back]
PFO
Closure - A Patent Foramen Ovale means a "hole"
between the right and left atrium. A patient who has
PFO has an increased chance of stroke. Drugs, such
as Coumadin (Warfarin), thin out the blood and assist
in the reduction of a clot returning to the right
atrium from the venous circulation in some patients.
Coumadin may lead to complications including internal
bleeding, cerebral bleeding, ulcers, hematuria, and
hemorrhoidal bleeding. It is recommended that PFO's
be closed in such patients particularly those with
mini-strokes(transient ischemic attacks or TIAs).
And, although traditional methods of closing PFO would
involve open-heart surgery, modern medicine and technological
advancements now make it possible to use special cardio
devises and new treatments in which recovery is quick
and the patient is discharged from the hospital in
less than 24 hours without the need to open the chest.
[back]
ASD
Closure - Atrial septal defects (ASD) are congenital
irregularities. When the opening between the wall
and the two atria or septum does not close at birth
as it is supposed to, the blood to bypass the lungs
does not occur correctly. The size of the ASD can
be very small or more than an inch in diameter. The
higher blood pressure in the left atrium pushes blood
into the right atrium, adding additional supply of
blood to the heart. This added volume increases both
the workload of the right ventricle and the flow of
blood in the lungs. Larger defects may cause symptoms
including shortness of breath, sweating a lot with
activity, increased breathing rate, or decreased growth.
Congestive failure may develop, with cough and swelling
of the legs and ankles. Occasionally, the added strain
on the heart results in irregular heart beats. Patients
who are found to have an ASD should have it closed.
In the past ASD closure required surgery, now ASD
closure is a "knifeless" procedure. This procedure
is very safe, and prevents the patient from suffering
blood clot and heart rhythm and pumping disturbances.
[back]
OUTPATIENT
PROCEDURES
Diagnostic
outpatient procedures, such as the one listed below
can detect medical conditions early to prevent cardiovascular
complications in the future, thus placing greater
emphasis on proper cardiac care. Early detection of
coronary, carotid, renal and peripheral artery blocklages
are extremely important in cardiovascular disease
prevention.
The following outpatient procedures are all performed
in exceptional well-equipped facilities along with
a highly qualified team of nurse/nurse practioners,
technicians and a medical support staff specifically
trained in cardiovascular care. Please contact our
team (link) directly with any questions and we will
be happy to assist you with any inquiries. Further
information regarding the following procedures, including
descriptions and pre and post procedural information
can be found on our site under Patient Information
(link) The highlighted outpatient procedures are the
most common and follow a text summary of the procedure.
If you would like more information on a specific procedure
that is not highlighted, contact our offices directly.
Outpatient
services include: (anchors)
Blood
tests (Lipids, C-Reactive
Protein, Homocysteine)
Nuclear Stress Testing
Carotid Duplex
Ultrasound
Vascular Duplex
Ultrasound
Echocardiogram
Blood
tests (Lipids, C-Reactive Protein, Homocysteine)
Lipoprotein(a):
Lipoprotein(a) or Lp(a) is an established risk predictor
for heart attack. It not only has a cholesterol component,
like LDL (bad lipid), but a pro-thrombotic (blood
clotting) component. Lp(a) levels are genetically
determined and remain relatively constant over an
individual's lifetime. Unfortunately, they are not
affected by lifestyle changes or by most drug therapy.
High Lp(a) levels increase the risk for developing
coronary artery disease as well as cerebral vascular
disease. Elevated levels of Lp(a) are thought to work
independently, to add to any underlying heart or vascular
disease processes.
High
Lp(a) levels can occur in individuals with normal
cholesterol levels; if so, they do not carry the same
cardiovascular risks as high Lp(a) levels in individuals
with high LDL levels. According to one review, the
relative risk of cardiovascular disease events attributable
to elevated Lp(a) is modest (2-fold increase) in subjects
with normal LDL cholesterol levels. However, subjects
with high LDL levels, such as those with familial
hypercholesterolemia who typically present with LDL
levels in the 300 mg/dL range, have a 12-fold increase
in the risk of heart attack attributable to concomitantly
high levels of Lp(a).
[back]
C-Reactive
Protein: The C-reactive protein (CRP) test is
a blood test that measures the level of CRP in the
blood. CRP is an inflammatory marker - a substance
that the body releases in response to inflammation.
High levels of CRP in the blood mean that there is
inflammation somewhere in the body. Other tests are
needed to determine the cause and location of the
inflammation. A test called "High Sensitivity CRP"
(HS-CRP) is done to distinguish between arthritis
inflammation and inflammation possibly related to
cardiovascular disease. Studies indicate that men
with high levels of CRP have triple the risk of heart
attack and double the risk of stroke compared to men
with lower CRP levels. In women, studies have shown
that elevated levels of CRP may increase the risk
of a heart attack by as much as seven times.
[back]
Homocysteine:
Homocysteine is an amino acid produced as a normal
byproduct of the breakdown of methionine (from proteins),
which is an essential amino acid acquired mostly from
eating meat. Studies have shown that too much homocysteine
in the blood is related to a higher risk of coronary
heart disease, stroke and peripheral vascular disease.
There's plenty of evidence that homocysteine can be
kept at moderate, healthy levels if the body has adequate
levels of three important B-vitamins: vitamin B-6,
vitamin B-12 and folic acid (the synthetic and more
easily absorbed version of folate). These B-vitamins
convert homocysteine into a harmless substance. However,
a lack of any of these three vitamins can increase
homocysteine levels, which could prove to be dangerous.
Consult your physician before taking these vitamins
because they could hide a B-vitamin deficiency, which
could lead to nerve damage. Some physicians routinely
screen for this deficiency before adding B-vitamins.
The
basic determination is that homocysteine is most likely
an independent risk factor for cardiovascular disease
but it's contribution is less then the major risk
factors. The major risk factors are smoking, diabetes,
high cholesterol and high blood pressure.
[back]
Nuclear
Stress Testing: Also known as "thallium or sestimibi
stress testing," this procedure is almost identical
to exercise stress testing. After the patient is attached
to an electrocardiogram (EKG) and a blood pressure
machine, exercise is started on a treadmill, a stationary
bicycle, or a stair machine. Nuclear stress testing
is performed to evaluate the condition of the heart
and the arteries that supply it. During exercise,
the heart has a greater need for blood and the oxygen
and other nutrients within it. If the coronary arteries
are partially or totally blocked, they will not be
able to meet that demand, creating a condition called
cardiac ischemia - inadequate blood supply to the
heart muscle. Monitoring the thallium blood flow in
the heart, and the amount of time that it remains
there, reveals abnormalities in the heart and coronary
arteries.
With
the nuclear test, a radioactive isotope, thallium
or sestimibi, is injected in an arm vein and the thallium
is absorbed into the heart muscle for several hours.
Scans are performed immediately after exercise and
several hours later to detect a lack of blood supply
to the heart. EKG electrodes are attached to the chest
and a blood pressure cuff is placed around the upper
arm. Depending on the patient's response to stress,
the test could last from one to 15 minutes. When the
doctor decides that the exercise stress has been sufficient,
the exercise machine is stopped, and an intravenous
injection of the radioactive material is given.
[back]
Carotid
Duplex Ultrasound: Carotid duplex is the use of
ultrasound -- high frequency sound waves -- to evaluate
blood flow in the carotid artery in the neck. It generates
a two-dimensional, black and white picture that shows
whether there are any blockages, such as atherosclerotic
narrowing or blood clots, in the carotid artery. The
carotid artery supplies blood to the brain. A carotid
duplex is performed to detect narrowings or obstructions
(such as clots) in the artery, which increases the
likelihood of stroke.
The
patient reclines on an examining table while the sonographer
moves the transducer wand slowly along the sides of
the neck. Images from the sound waves will appear
on a video screen that the sonographer views during
the process. Total time is between 15 and 30 minutesThe
sonographer applies a cool, colorless gel to the neck
and to the tip of the sonography wand (transducer).
The wand is gently rubbed across the patient's neck.
Sounds from the movement of blood and images of the
blood flow in the artery are generated. The test is
non-invasive and painless.
[back]
Vascular
Duplex Ultrasound: Vascular Doppler is performed
to detect obstructions in the leg arteries. These
obstructions may be causing symptoms, such as leg
pain when walking or doing other forms of exercise.
Vascular
Doppler, also known as an arterial ultrasound, uses
two techniques to evaluate the blood pressure and
blood flow in the arteries in your legs. These techniques
are blood pressure measurement using cuffs similar
to those used for arm measurements of pressure, and
ultrasound (high frequency sound waves). Essentially,
a sonography wand replaces the stethoscope normally
used when blood pressure is taken. The process generates
pressure measurements and images that show whether
there are any blockages in the leg arteries. Blood
pressure measured in the legs should be similar to
that taken in the arms; if it is lower, it may signal
the development of atherosclerotic plaque in your
arteries that is interfering with the circulation.
The
sonographer wraps a blood pressure cuff around the
patient's leg at four or five locations. Then a cool,
colorless gel is applied to the top of the foot and
to the tip of the sonography wand (transducer). The
wand detects blood pulses as the blood pressure cuffs
inflate and deflate. Total time for the test is between
45 minutes and an hour. The test is totally non-invasive.
There is no post-procedural care and the patient may
leave immediately after the test. In cases when leg
pressures need to be checked both before and after
exercise, the patient is asked to walk on a treadmill
for a short time before the pressure measurements
are repeated.
[back]
Echocardiogram:
Also known as: echo, 2D echo, cardiac ultrasound,
cardiac sonogram. An echocardiogram is an imaging
procedure that uses high frequency sound waves to
provide a picture of the heart's movement, valves,
and chambers. It may be combined with a Doppler ultrasound
and color Doppler to evaluate blood flow through the
heart's valves. An echo reveals the size and shape
of the heart, and its chambers. It can provide information
about disease of the muscle and valves, and can help
identify tumors and congenital heart disease. It also
assesses the pumping function of the heart, yielding
a number called the ejection fraction. (A normal EF
is 55 to 80%; lower numbers reveal some level of impaired
pumping.)
A
cool, colorless gel is applied to the chest and to
the tip of the wand held by the cardiac sonographer.
(The wand looks like a small microphone.) The wand
is gently rubbed across your chest. A gentle pressure
is felt from the wand, but there is no pain. During
a Doppler procedure, dull thumping sounds may be heard.
These sounds are normal and are produced by the movement
of blood through various vessels.
-
The patient is asked to remove all clothing and jewelry,
from the waist to the neck, and given a hospital gown.
- The sonographer places three electrodes on the chest,
using small sticky patches. These electrodes are attached
by wires to an electrocardiograph monitor to generate
an electrocardiogram (ECG) - a record of the heart's
electrical activity.
- The patient lies on his left side on an exam table.
- The sonographer applies a small amount of cool gel
to the chest and to the sound-wave transducer at the
tip of the wand. The gel helps assure good contact
and clearer pictures.
- The sonographer moves the wand slowly around the
chest.
- The patient is asked to change position, from the
back to the side, to provide different visual angles.
The patient will also be asked to hold his breath
briefly during some parts of the procedure.
- The sonographer watches the images on a screen during
the procedure, and a permanent record of the images
also is made.
- Depending on the extent of the procedure, it may
take anywhere from 30 to 60 minutes.
There
is no post-procedural care and no risks to the procedure.
After the procedure, the sonographer wipes the gel
from the chest and the patient may dress and leave.
[back]
|